| |
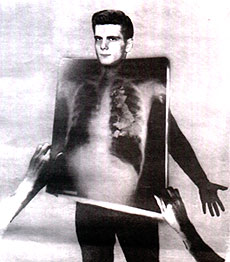
TB, that
‘quiet and solemn struggle between soul and
body’, is on the rise again, NIGEL HAWKES reports
For
a century or more, a pilgrimage of death saw thousands
of English consumptives making their painful journey
to Pan, a small French town in the shadow of the
Pyrenees. Here, they believed, a climate of tranquillity
could free them from a disease that already had
them by the throat.
The winter trees in Pan might
tremble, but they would never shake. The town
was calm, its gardens handsome, its air as still
as a shroud. To generations raised in the belief
that wind, chill and the bustle of cities were
the enemies to be avoided, Pan represented hope.
It is easy to mock the false
expectations, but impossible not to be moved by
the hopes that Pan inspired. Tuberculosis was
a terror without class distinction. Nobody knew
how it was caused, how it chose its victims. When
a lifebelt is nowhere to be found, grasping at
a straw makes a kind of sense.
Professor Charles Louis,
France's leading TB expert in the 1840s, married
late. When TB struck down his only son, Louis
gave up his career and went to live with him in
Pan. He did not believe that a change of climate
could effect a cure, and never changed his mind.
But he went on hoping against belief, a mental
contortion of the kind TB imposed even upon the
most rational. His son soon died.
In
the first half of the 19th Century there was hardly
a person in London who was not infected with TB.
But while infection was universal, the disease
was not. Even though it was the principal cause
of death in Europe and much of North America,
its incidence had an arbitrariness that puzzled
even the cleverest physicians.
We now know that TB is caused
by a bacillus, a rod-shaped bacterium first isolated
by the German Robert Koch in 1882. But not all
those who carry the bacillus develop the disease.
In an era when everybody was exposed to TB it
was perfectly sensible to believe that the disease
was hereditary, since what determines illness
in such circumstances is genetics. If everybody
carries a germ but only a proportion succumb,
then it is the genes that pick losers from winners.
In 1837 the English physician
Sir James Clerk listed "improper diet, impure
air, deficient exercise, excessive labour, imperfect
clothing, want of cleanliness, abuse of spirituous
liquors, mental causes and contagion" as
the causes of consumption. The germ came last
in Sir James' catalogue.
 |
| 1936: At St. Thomas' hospital,
TB patients take to the open air |
His contemporary, the American
physician William Beach, dismissed contagion altogether,
emphasising instead hereditary disposition"
marked by such features as a narrow chest or prominent
shoulders. Beach recommended travel, sending a
few more American consumptives to the grand hotels
of Pan and others to Brazil and the West Indies.
Beach was wrong, but so perhaps
were those who saw Koch's discovery as "the
last word on the subject". The historiography
of TB is split by a long-running and fascinating
dispute over how it came to be conquered, a dispute
that is of more than merely historical interest
now that TB is on the march again.
If the bacillus is the villain,
then it is the sulphonamides and, later, the antibacterials
that are the heroes of the TB story. By identifying
a germ, Koch set in train the process that in
due time produced the magic bullets to destroy
that germ, and eliminate the disease.
But the paradox is that TB
was on the wane by the time the magic bullets
arrived. It had been in steady - indeed, precipitate
- decline since the 1840s, for reasons still argued
over. The historian Thomas McKeown has claimed
that TB and other infectious diseases declined
not as a result of medical interventions but in
consequence of social and economic changes.
"Effective clinical
intervention came late in the history of the disease,
and over the whole period of its decline the effect
was small in relation to that of other influences,"
he said. Better nutrition was the key, according
to this view.
One could equally argue that
the germ itself had changed, or that better public
hygiene and the isolation of infective TB patients
had made the difference. The fact remains that
TB was on the way to being conquered before doctors
had the weapons to which their victory is now
attributed. Other nightmare diseases have seen
a similar rise and fall in incidence: today the
parallel is with heart disease, whose decline
is difficult to explain by the dietary theories
supposed to be its cause.
Misunderstanding what put
paid to TB is a major part of the problem we have
with the disease today. The theory that drugs
had conquered infection had only brief prominence,
from about 1960 to the appearance of HIV infection
in the early 1980s, but most of today's doctors
took it in with their mothers' milk. What was
overlooked was the germ's capacity to change in
response to a new environment, and its ability
to prey on those weakened by AIDS, poverty and
neglect. To have ignored some of these things
required averting the gaze from what has been
going on in the Third World, but we are well practised
in that art. It was much easier to see the rise
of TB among the poor as the failure of governments
to deliver the drugs needed to control it.
 |
Compliance - or the lack
of it - became the World Health Organisation's
watchword, its policy one of directly observed
therapy, or standing over people making sure they
took their pills. There is nothing wrong with
this, as far as it goes. But curing even a standard
case of TB requires compliance over many months,
and drug-resistant TB is a tougher problem still.
Multidrug-resistant TB (MDR-TB) can be treated,
but only at huge cost.
In New York, where valiant efforts have been made
to get MDR-TB under control, management of a single
case can cost US$250,000. In Russian prisons,
where TB is rife, a fifth of all cases - some
say two fifths - are estimated to be MDR-TB.
Nor has the rise of TB left
its old stamping ground untouched. The teeming
slums of London in the 19th Century provided an
ideal culture medium for multiplying TB. Today,
London is much cleaner and less crowded, but TB
infections are nevertheless on the rise once more.
The rate of infection in Newham, at 100.6 per
100,000, is now greater than it is in Uzbekistan
(94 per 100,000) or Azerbaijan (82).
The whole of this increase
can be accounted for by the poorest 30 per cent
of society, especially those who live in crowded,
ethnically diverse communities where immigration
is a major source of new infection. The rich have
as yet no need to fear TB as they once did, but
the rise in cases has not yet elicited the kind
of response in London that turned the tide in
New York.
Nor has basic protection against TB been stepped
up. While cases have been rising, vaccination
has fallen, from 742,000 in 2001-02 to only 450,000
in 2002-03. The risk of catching TB in the shires
may still be very low, but there is little evidence
of any concerted effort to keep it that way. Like
doctors, ministers seem locked in a simplistic
model of how TB was conquered, and persistently
make public health a far lower priority than efforts
to improve hospital care or deliver drugs.
But the real lesson of TB
is more profound than quibbling about whether
the British government, or any overnment, is doing
enough to deal with it. Rather, as Alimudden Zumla
and Matthew Gandy argue in a new book, The Return
of the White Plague, it is a question of explaining
how a deadly disease that has a cheap and effective
cure remains the leading cause of death and disability
worldwide.
This is, they insist, a medical
failure. How can it be that in 1993, more than
50 years after the development of effective treatments,
the World Health Organisation was forced to declare
TB a global emergency?
This is, said Charles Dickens,
"a dread disease, in which the struggle between
soul and body is so gradual, quiet and solemn,
and the result so sure, that day by day and grain
by grain the mortal part withers away, so that
the spirit rows light and sanguine with its lightening
load and, feeling immortality at hand, deems it
but a new term of mortal life - a disease in which
death takes the glow and hue of life, and life
the gaunt and grisly form of death".
That is the kind of prose
we need to wake us to a threat that once sent
thousands to die in Pan. We conquered TB once;
now we need to do it again.
- The Times |
|

